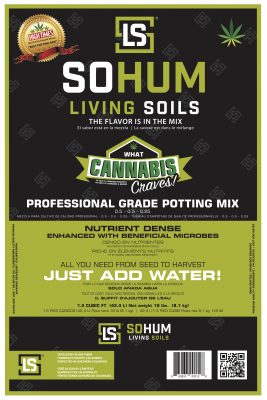
Check our line of indoor and outdoor grow supplies - Roots Organics lush Soils, FoxFarm, and Black Gold soils, organic nutrients, coco coir and general hydroponic systems. Shop for Led Lighting, Dehumidifiers, AC Infinity products, Flora Flex and more! It's all here! Come visit our St. Louis Hydroponic garden center at 8445 Natural Bridge Rd. in St. Louis, Mo. 63121
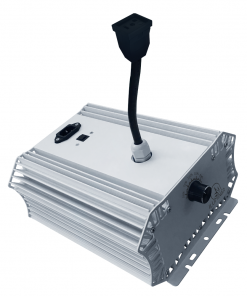
Accessories
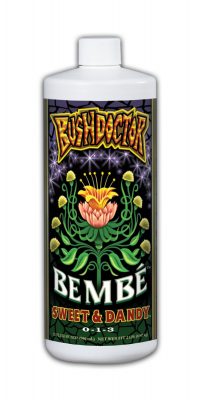
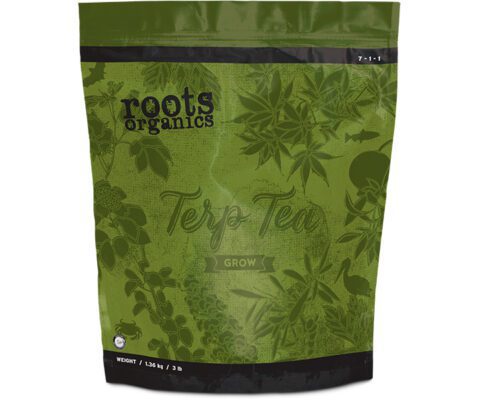
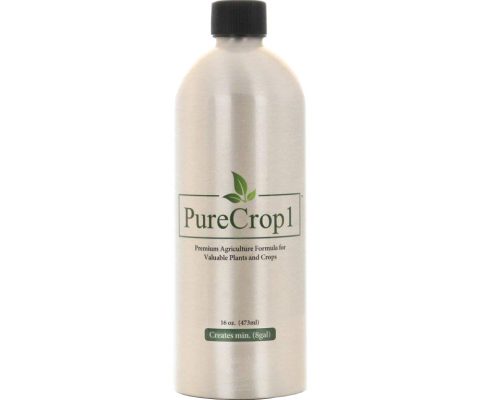
Nutrients & Additives
Nutrients & Additives
Hydro Systems
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Hydro Systems
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Hydro Systems
Hydro Systems
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
LED Lighting
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Nutrients & Additives
Get ready for the fall season now. The grow generation is here and they are growing some of the best food and herbs. Search above, its all here! Start your grow with a clone dome, and complete hydroponics systems. Bloom Boosters, Super Thrive, Trimmers, Trellis Nets, Drying Nets, and Trim Bins. These are just few items to start the fall off right! Can't find it? Give us a call at 314-265-1330.
Pots & Containers
Growing Media
Pumps & Irrigation
Pots & Containers
Nutrients & Additives
Garden Accessories
Growing Media
Nutrients & Additives
Fluorescent Lighting
Pots & Containers
Dirt Pot Flexible Portable Planter, Grey, 5 gal, with handles
Food Storage
Fluorescent Lighting
Pots & Containers
Nutrients & Additives
Nutrients & Additives
Garden Accessories
Fluorescent Lighting
Jump Start T5 Strip Fixture Link Cord, For Modular Systems, 21″
Pots & Containers
Accessories
Pots & Containers
Seed Starting
Plant Care
Tents & Tarps
Pots & Containers
Dirt Pot Flexible Portable Planter, Grey, 10 gal, with handles
Nutrients & Additives
Fluorescent Lighting
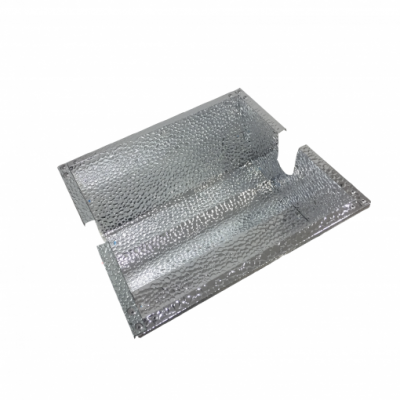
Grow Light Reflectors
Pumps & Irrigation
Click on these categories for Climate Controllers, grow lights, timers, hydro systems, PH Meters, intake filters, nutrients and garden accessories
Order with Confidence
Most orders are shipped with in 24 hours. Signup and become a Loudbank Member and receive discounts and points on future purchases. Items are dispatched from the US and will arrive in 5-7
days.
Amazing customer service
Our knowledgable team is dedicated to providing quality equipment to commercial and residential growers with the need to ensure that their operations are operating with maximium efficiency, output and quality.
Purchasing Convenience
Serving the U.S. and Canada. We accept all major credit cards including Visa, Mastercard, American Express, Discovery and PayPal.
COVID-19 DISCLAIMER
For your safety and that of others, LoudBank Garden Supplies is adhering to all regulations and guidelines from government authorities related to containment of COVID-19. Please be advised that there may be significant delays for customer deliveries as a result of these issues beyond our control.